At The Green House Surgery we take patient safety very seriously. We follow the latest advances in medical research and continually update and review our clinical practice to ensure patient care is of the highest standard.
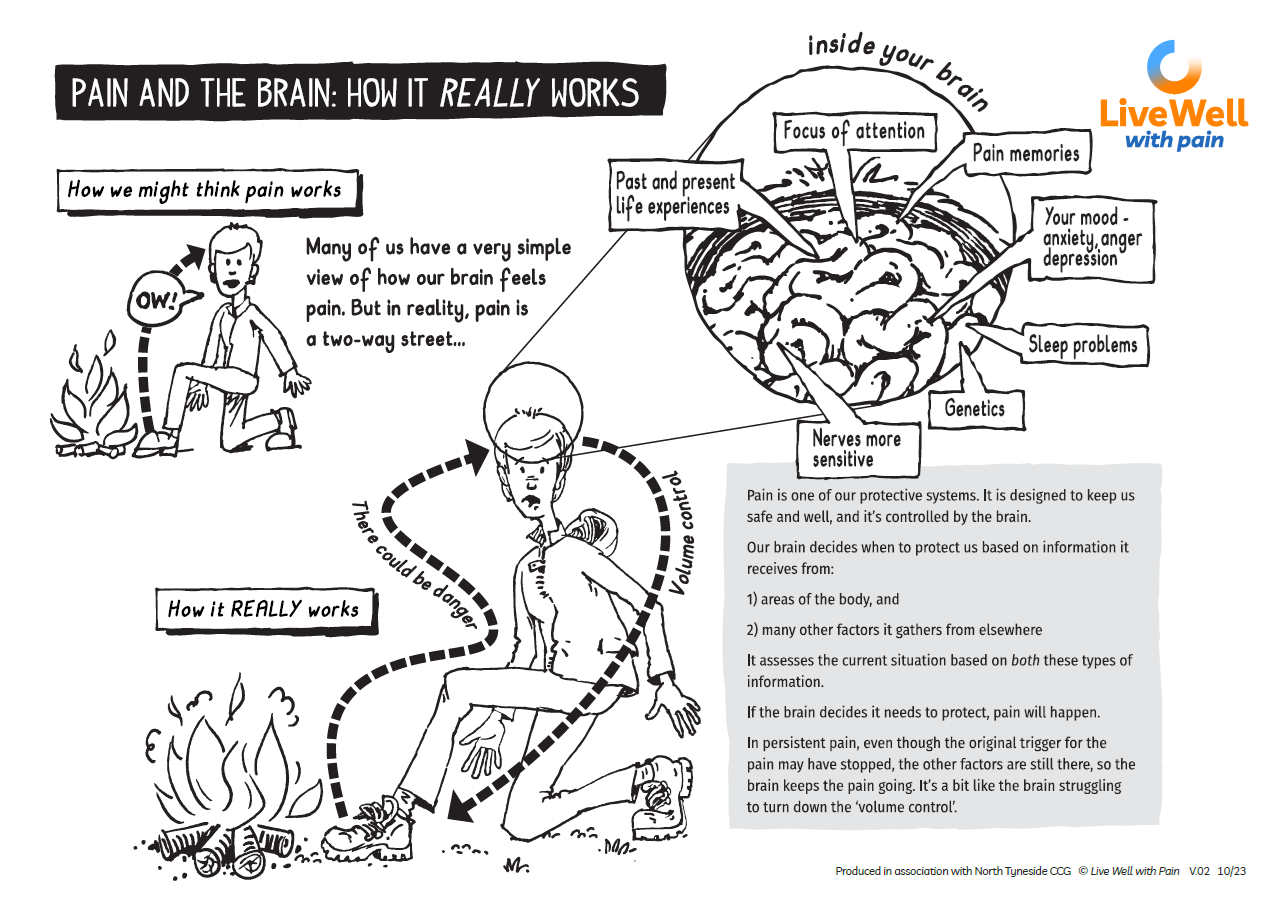
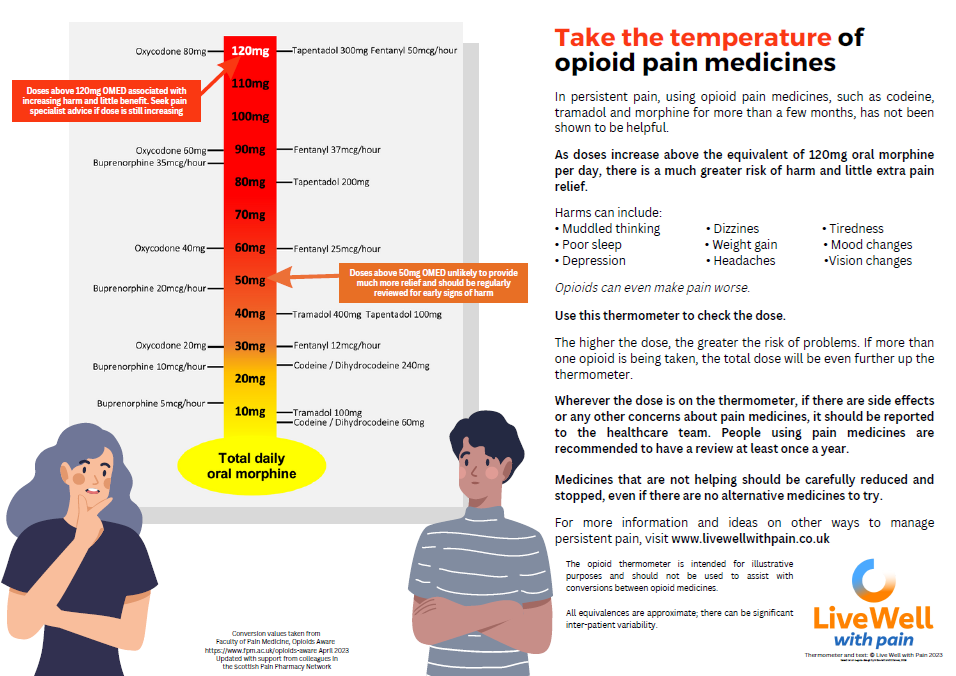
Recent research has highlighted a significant risk to patient safety around the use of opioid type painkillers for chronic pain. We know that these drugs are helpful in pain of recent onset such as a broken bone and they are also effective in patients with cancer related pain.
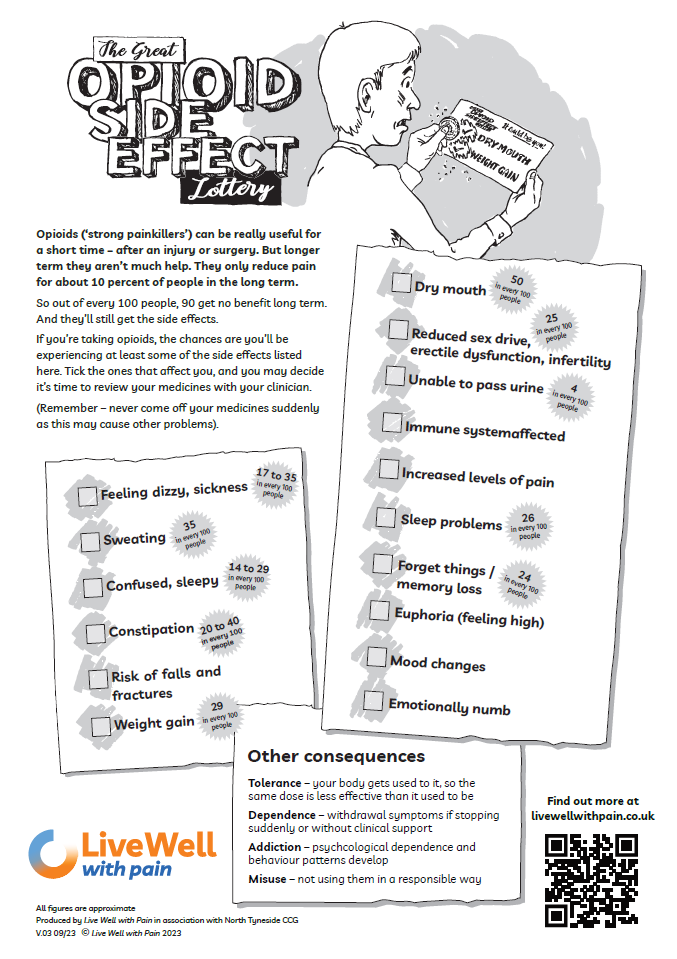
However, recent medical evidence questions the benefit of opioid type painkillers for chronic (lasting more than a few months) pains. There is now better understanding of the risks, including:
- reduced fertility/sex drive/erectile dysfunction in men or irregular periods in women
- reduced ability to fight infection
- increased levels of pain
- dependence
- breathing issues (respiratory depression)
Therefore, we are starting to review those who are on long-term pain killers (including opiates) and we would like to support you to reduce the amount you take. It is important these medicines are not stopped suddenly which can cause withdrawal side effects so we will support you to reduce slowly over time.
If this is a service you are interested in accessing, please contact the practice and ask to be booked into our opioid reduction clinic.